Alpha-1 Antitrypsin Deficiency
Alpha-1 antitrypsin (AAT) deficiency is a rare disorder caused by mutations in the SERPINA1 gene, which encodes the AAT protein. The disorder can lead to hepatic or pulmonary disease. Although several therapies are currently available for the management of lung complications, there are no available therapies specifically for AAT deficiency-associated liver disease (AATLD).
Function of AAT protein and its relationship to liver disease
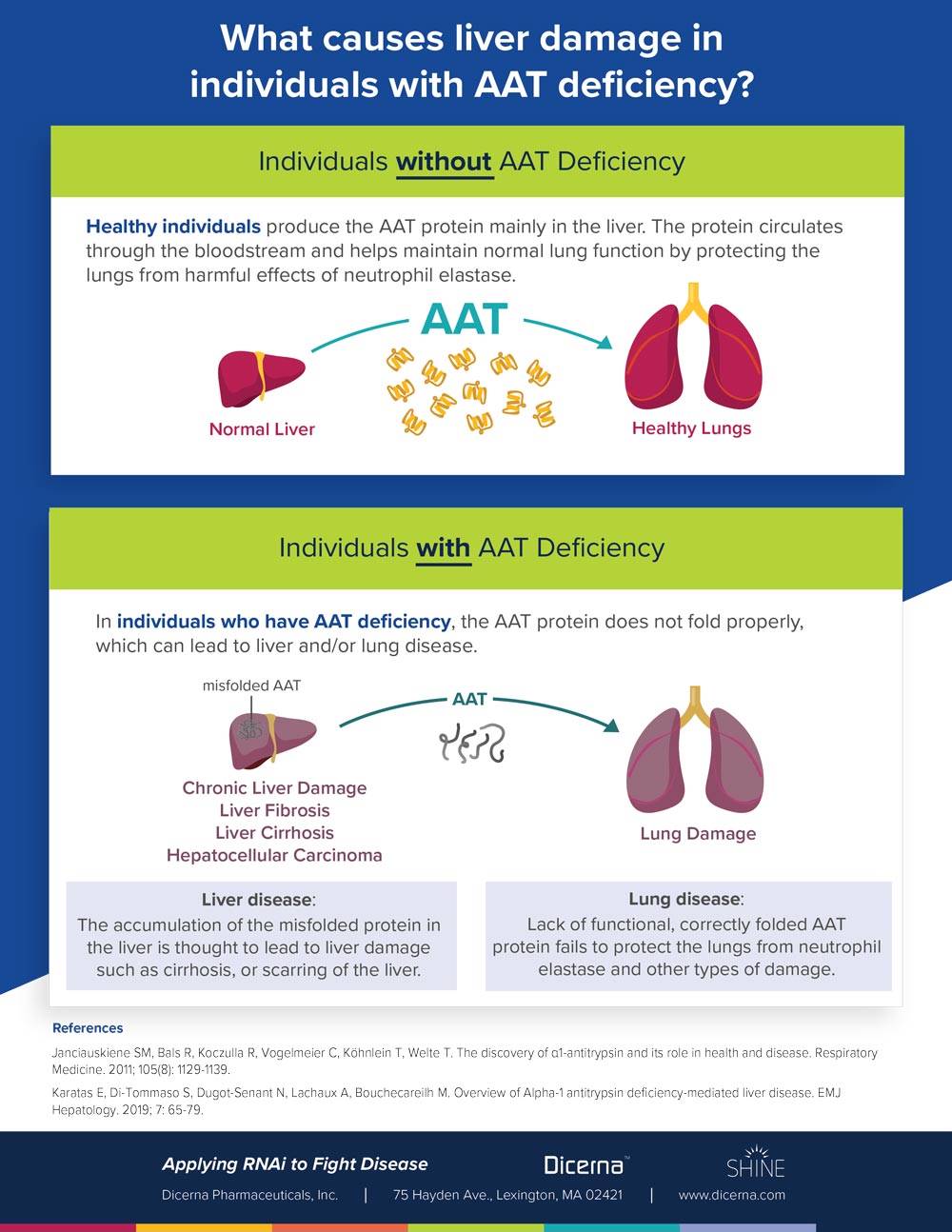
AAT is a soluble plasma protein synthesized and secreted primarily by hepatocytes. Polymerization and aggregation of the misfolded AAT protein in hepatocytes can inhibit secretion of AAT protein into the bloodstream. Toxic accumulation of mutant AAT in the liver may lead to liver disease.
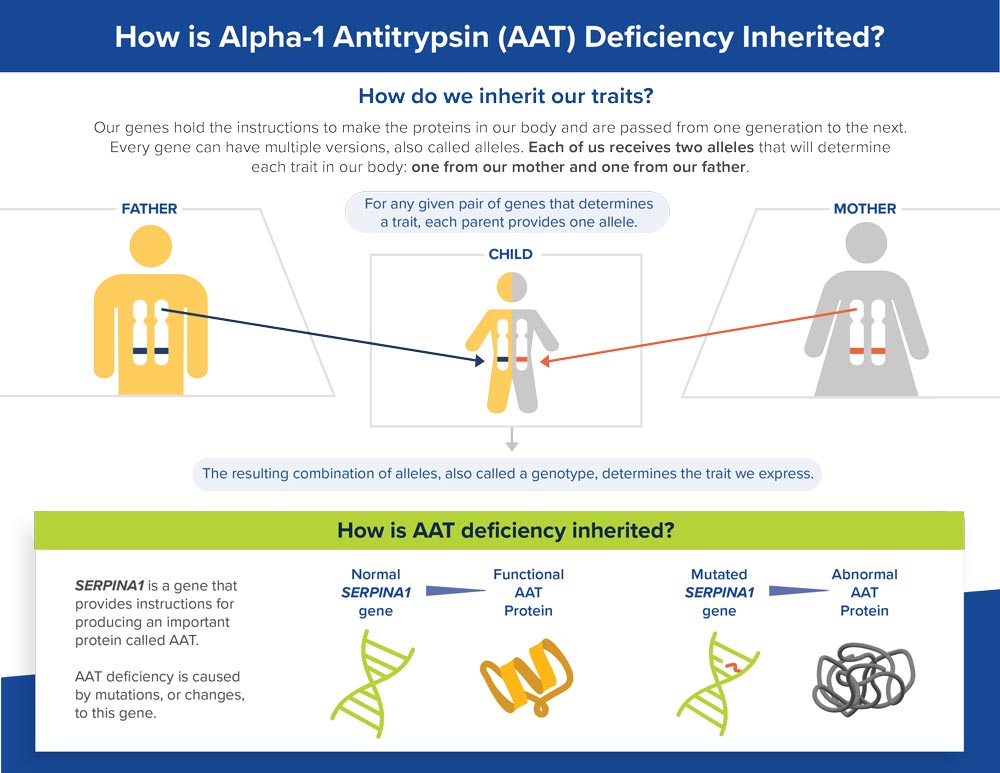
Cause
AAT deficiency is caused by mutations in the SERPINA1 gene, which encodes AAT protein. AAT protects the lungs and other parts of the body by neutralizing neutrophil elastase, an enzyme that fights infection but can also attack normal tissues if not adequately regulated by AAT. Mutated versions of the SERPINA1 gene result in production of misfolded AAT protein. Lack of functional, correctly folded AAT protein fails to protect the lungs from neutrophil elastase and other types of damage. The malfunctioning AAT protein accumulates in the liver and is thought to lead to liver damage and resulting disease, including complications such as cirrhosis.
The majority of individuals with AATLD express an autosomal mutant Z-allele (PiZ) containing a Glu342Lys missense mutation in SERPINA1 as homozygosity (PiZZ genotype). Individuals with other mutated alleles, such as the mutant S-allele (PiS), leading to the PiSZ or PiSS genotype, may also develop liver or lung disease, but at a lower frequency.
Symptoms
The clinical presentation and course of AAT deficiency are highly variable, in both liver and lung disease.
Liver disease
The symptoms of AATLD can appear as early as infancy or occur later in adulthood. A small percentage (approximately 5%) of children with AAT deficiency may face life-threatening liver disease within the first few years of life.
Symptoms include:
- Jaundice
- Itching
- Fatigue
- Swelling of the liver and spleen
- Portal hypertension (increased blood pressure in blood vessels that lead to the liver)
- Hepatosplenomegaly (abnormal swelling of the liver and spleen)
- Ascites (swelling of the abdomen due to fluid buildup)
- Intestinal bleeding
- Poor weight gain, growth and failure to thrive in infants and children
In addition to the above symptoms, individuals of all ages can have fibrosis (scarring) and abnormal liver function tests, which measure levels of liver enzymes in the bloodstream.
Some individuals may develop necrotizing panniculitis, or the formation of painful ulcers under the skin, leading to breakdown of tissue. In addition, children and adults with AATLD may develop liver cirrhosis, and adults may develop hepatocellular carcinoma (HCC).
The only cure for AATLD is a liver transplant. In a systematic review of 35 papers reporting treatment outcomes (28 papers in children, 7 papers in adults), 7.5% of children with AAT deficiency were reported to develop cirrhosis, and 16.5% of pediatric patients required a liver transplant; among adults, 10.5% had liver cirrhosis, and 14.7% required a liver transplant.
Lung disease
AAT deficiency is associated with development of chronic obstructive pulmonary disease (COPD), which usually manifests as small airways disease and emphysema. Individuals who smoke are at increased risk of developing lung disease. Augmentation therapy with an alpha-1 proteinase inhibitor, which requires weekly intravenous (IV) infusion, is standard therapy in some countries for patients with AAT deficiency-associated emphysema.
 Prevalence
Prevalence
More than 95% of all individuals who are severely AAT-deficient have either the PiZZ or PiSZ genotype. In most cases, individuals with AAT-associated liver disease have the PiZZ genotype.
Recent epidemiological studies estimate the worldwide prevalence of PiZZ genotype at more than 250,000 individuals.
- 120,000 in Europe
- Nearly 74,000 in North America, including roughly 63,000 in the U.S.
- The incidence of this genotype is highest in people of Northern European descent
The proportion of adults with the PiZZ genotype who will develop liver disease is not clear. Risk factors associated with development of liver disease include age over 50 years, male gender, repeated elevated liver enzymes, hepatitis virus infection and presence of diabetes mellitus or COPD. Individuals with other genotypes may develop liver or lung disease, but the prevalence is not well known.
Diagnosis
The diagnosis of AAT deficiency-associated liver or lung disease is essentially a diagnosis of exclusion. Current guidelines recommend testing all individuals with COPD and/or unexplained liver disease for AAT deficiency. Individuals with necrotizing panniculitis, granulomatosis with polyangiitis, or unexplained bronchiectasis should also be tested for AAT deficiency. The guidelines recommend genotyping to test for S and Z alleles, noting that the specificity and sensitivity of current genotyping panels for these alleles exceed 99%. More advanced testing methods may include proteinase inhibitor (Pi) typing, AAT genotyping and expanded genotyping for rare alleles and gene sequencing. Serum AAT levels alone are not sufficient for diagnosis because AAT levels can fluctuate due to a number of factors, including inflammation, infection and injury.
Many individuals with AAT deficiency experience long delays between the appearance of first symptoms and diagnosis. Early studies estimated an average diagnostic delay of 7.2 years. An analysis of the diagnosis experience of 1,020 symptomatic individuals with AAT deficiency reported an average interval of 8.3 ± 6.9 years between the onset of pulmonary symptoms and diagnosis, and an average of 2.7 ± 2.4 physicians seen before individuals received a correct diagnosis.
Treatment
Currently, there are no available therapies specifically designed to treat AATLD. Healthcare providers generally offer standard liver supportive care such as ursodeoxycholic acid to manage the complications of chronic liver disease. Individuals with severe, life-threatening liver disease may undergo a liver transplant, which is associated with excellent success rates, as AAT protein levels typically return to normal following transplantation.
For more information about Dicerna’s clinical trial for AATLD, visit: clinicaltrials.gov using the identifier NCT04764448.
The Impact of AAT Deficiency
Individuals with PiZZ genotype may experience a shortened lifespan due to the complications of liver or lung disease. In a cohort analysis of individuals with liver disease in the Swedish National AATD Register, 106 (68%) of 155 subjects died during follow up; causes of death included liver failure, HCC, cardiovascular disease, gastrointestinal bleeding, respiratory failure, and peritoneal abscess. The probability of death within one year after onset of liver disease is 45%. The potential for severe outcomes associated with AATLD underscores the urgent need for therapeutic options for individuals with this condition.
References
- National Institutes of Health, U.S. National Library of Medicine, Lister Hill National Center for Biomedical Communications. Genetics Home Reference: Alpha-1 Antitrypsin Deficiency. https://ghr.nlm.nih.gov/condition/alpha-1-antitrypsin-deficiency. Published Sept. 2019. Accessed Jan. 2020.
- Janciauskiene SM, Bals R, Koczulla R, Vogelmeier C, Köhnlein T, Welte T. The discovery of α1-antitrypsin and its role in health and disease. Resp Med. 2011; 105(8): 1129-1139.
- Zuo L, Pannell BK, Zhou T, Chuang CC. Historical role of alpha-1-antitrypsin deficiency in respiratory and hepatic complications. Gene. 2016; 589(2): 118-122.
- American Thoracic Society; European Respiratory Society. American Thoracic Society/European Respiratory Society statement: standards for the diagnosis and management of individuals with alpha-1 antitrypsin deficiency. Am J Respir Crit Care Med. 2003; 168(7): 818-900.
- Karatas E, Di-Tommaso S, Dugot-Senant N, Lachaux A, Bouchecareilh M. Overview of Alpha-1 antitrypsin deficiency-mediated liver disease. EMJ Hepatology. 2019; 7: 65-79.
- De Serres F, Blanco I. Role of Alpha-1 antitrypsin in human health and disease. Journal of Internal Medicine. 2014; 276: 311-335.
- Patel D, Teckman J. Alpha-1 antitrypsin deficiency liver disease. Clinical Liver Disease. 2018; 22: 643-655.
- Crystal RG, The alpha-1-antirypsin gene and its deficiency states. Trends in Genetics. 1989; 5(12): 411-417.
- Blanco I, Bueno P, Diego I, et al. Alpha-1 antitrypsin Pi*SZ genotype: estimated prevalence and number of SZ subjects worldwide. Int J Chronic Obstr Pul Dis. 2017; 12: 1683-1694.
- Teckman JH. Liver disease in alpha1-antitrypsin deficiency: Current understanding and future therapy. COPD. 2013; 10(S1): 35-43.
- Townsend SA, Edgar RG, Ellis PR, Kantas D, Newsome PN, Turner AM. Systematic review: the natural history of alpha‐1 antitrypsin deficiency and associated liver disease. Aliment Pharmacol Ther. 2018; 47(7): 877-885.
- Dunlea DM, Fee LT, McEnery T, McElvaney NG, Reeves EP. The impact of alpha-1 antitrypsin augmentation therapy on neutrophil-driven respiratory disease in deficient individuals. J Inflamm Res. 2018; 11: 123-134.
- Alpha-1 Foundation. Lung Disease. https://www.alpha1.org/Newly-Diagnosed/Learning-about-Alpha-1/Lung-Disease. Published 2019. Accessed Jan. 2020.
- Sandhaus RA, Turino G, Brantly ML, et al. The diagnosis and management of alpha-1 antitrypsin deficiency in the adult. Chronic Obstr Pulm Dis. 2016; 3(3): 668-682.
- Blanco I, Bueno P, Diego I, et al. Alpha-1 antitrypsin Pi*Z gene frequency and Pi*ZZ genotype numbers worldwide: an update. Int J Chronic Obstr Pul Dis. 2017; 12: 61-569.
- Tanash H, Piitulainen E. Liver disease in adults with severe alpha-1-antitrypsin deficiency. J Gastroenterol. 2019; 54: 541-548.
- Sanders CL, Ponte A, Kueppers F. The effects of inflammation on alpha 1 antitrypsin levels in a national screening cohort. COPD. 2018; 15(1): 10-16.
- Stoller JK. Alpha-1 antitrypsin deficiency: An underrecognized, treatable cause of COPD. Cleve Clin J Med. 2016; 83(7): 507-514.
- Campos MA, Wanner A, Zhang G, Sandhaus RA. Trends in the diagnosis of symptomatic patients with α1-antitrypsin deficiency between 1968 and 2003. Chest. 2005; 128: 1179-1186.
- Larsson C. Natural history and life expectancy in severe alpha-1 antitrypsin deficiency, Pi Z; Acta Medica Scandinavica. 1978; 204: 345-351.