What is alpha-1 antitrypsin (AAT) deficiency?
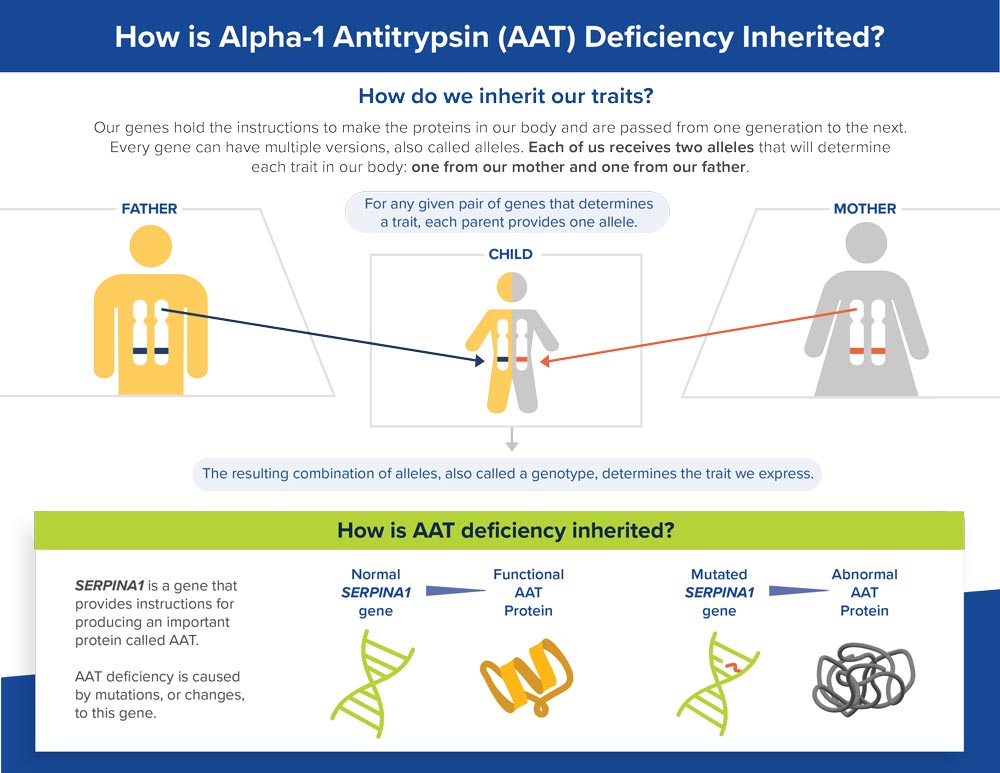
Alpha-1 antitrypsin (AAT) deficiency is a rare, inherited disorder that can lead to liver disease in children and liver and lung disease in adults. Despite progress in the development of treatments for lung complications, there are no available therapies specifically for AAT deficiency-associated liver disease (AATLD).
AAT deficiency is characterized by abnormally low levels of AAT protein.
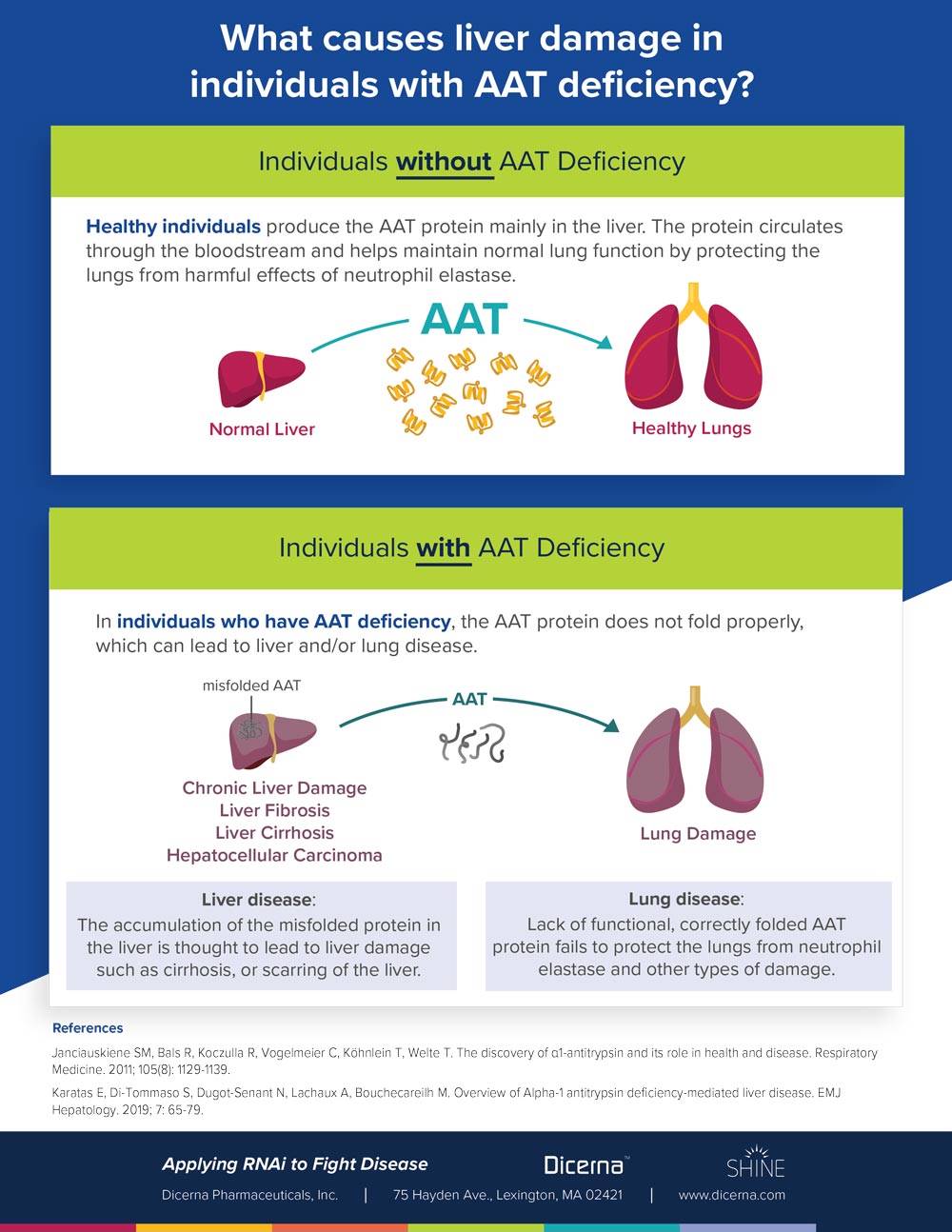
- In healthy individuals, the liver produces AAT protein and it circulates through the bloodstream and helps maintain normal lung function. AAT also contributes to other important functions in the body.
- In people with AAT deficiency, the liver produces an abnormal version of the AAT protein that clumps together and gets trapped in the liver, which can lead to liver damage. Because the AAT protein gets trapped in the liver, it does not circulate in adequate amounts in the bloodstream, which can lead to lung problems.
What is the cause of AAT deficiency-associated liver disease?
What is the purpose of AAT protein in the body?
Normally, the AAT protein protects the lungs and other parts of the body from a powerful enzyme called neutrophil elastase, which fights infection but can also attack normal tissues if it is not controlled by AAT.
What happens when the AAT protein is abnormal?
Mutated versions of the SERPINA1 gene result in production of abnormal AAT protein that does not fold properly. The accumulation of abnormal AAT in the liver is thought to lead to cirrhosis, scarring of the liver, and other types of liver damage. Additionally, lack of functional, correctly folded AAT protein fails to protect the lungs, leaving them vulnerable to damage from neutrophil elastase and other types of damage, such as from smoking and environmental toxins.
AAT deficiency may be associated with a range of liver and/or lung complications.
Liver
- Fibrosis, or the initial formation of scar tissue in the liver
- Cirrhosis, or widespread scarring of the liver
- Hepatocellular carcinoma (HCC), the most common type of primary liver cancer
Lung
- Chronic obstructive pulmonary disease (COPD)
- Emphysema
- Bronchiectasis, or thickening of the walls of the bronchi from inflammation or infection
What are the symptoms of AAT deficiency-associated liver disease?
Individuals with AAT deficiency can have symptoms of liver disease, lung disease, or both. The symptoms of AATLD can appear as early as infancy or occur later in adulthood.
Symptoms include:
- Jaundice (yellowing of skin and eyes)
- Itching
- Fatigue
- Swelling of the liver and spleen
- Portal hypertension (increased blood pressure in blood vessels that lead to the liver)
- Hepatosplenomegaly (abnormal swelling of the liver and spleen)
- Ascites (swelling of the abdomen due to fluid buildup)
- Intestinal bleeding
- Poor weight gain, growth and failure to thrive in infants and children
In addition to the above symptoms, individuals of all ages can have fibrosis (scarring) and abnormal liver function tests, which measure levels of liver enzymes in the bloodstream.
Who is at risk for AAT deficiency-associated liver disease?
Researchers estimate that more than 250,000 people around the world have the pair of gene variants called “ZZ.” This is the specific pair that most commonly leads to AATLD. Although most individuals with this pair will not develop liver disease, some will.
AAT deficiency occurs most frequently among people of Northern European descent
 How is AAT deficiency diagnosed?
How is AAT deficiency diagnosed?
If a healthcare provider suspects that an individual may have AAT deficiency based on their health history and other factors, he or she may order a genotype test to help diagnose AAT deficiency. This is a test that determines whether a person has the variant gene combination associated with increased risk of AAT deficiency. The provider can also check levels of AAT in the blood, as well as order specific tests to assess liver or lung function, depending on an individual’s specific symptoms.
For assessing liver function, the provider can order bloodwork to measure liver enzyme levels or can examine the liver via ultrasound or other imaging techniques such as computed tomography (CT) scanning. In some cases, a physician may order a biopsy to understand the extent and severity of liver disease.
Who should be tested?
Current guidelines recommend that anyone with COPD or unexplained liver disease should be tested for AAT deficiency. Family members of individuals known to have an abnormal gene for AAT should also be tested and provided with genetic counseling.
How is AAT deficiency-associated liver disease treated?
There are no available therapies specifically designed to treat AATLD. Several treatments are currently availble for individuals with AAT deficiency that affects the lungs. Healthcare providers generally offer supportive care to help patients manage their liver disease symptoms.
Some individuals with AATLD will require a liver transplant, after which AAT protein levels typically return to normal. Transplantation is currently the only effective therapeutic approach for AATLD. However, at present, liver transplantation fails to meet the needs of many individuals with this condition.
- Liver transplant surgery carries a risk of significant complications
- Individuals who undergo transplantation must take drugs to suppress their immune system for the rest of their lives, which can cause a number of side effects and increase risk of infection
- Individuals may not be eligible for transplantation if they are not healthy enough to undergo the surgery or tolerate the required lifelong medications
- The number of individuals in need of a liver transplant greatly exceeds the number of donor livers available for transplant
For more information about Dicerna’s clinical trial for AATLD, visit: clinicaltrials.gov using the identifier NCT04764448.
What is the Impact of AAT Deficiency?
Many patients with AAT deficiency require extended medical monitoring and treatment. Individuals with the “ZZ” gene combination may have a shortened lifespan due to serious complications of the disease, such as COPD (especially if they smoke) or liver failure.
References
- National Institutes of Health, U.S. National Library of Medicine, Lister Hill National Center for Biomedical Communications. Genetics Home Reference: Alpha-1 Antitrypsin Deficiency. https://ghr.nlm.nih.gov/condition/alpha-1-antitrypsin-deficiency. Published Sept. 2019. Accessed Jan. 2020.
- De Serres F, Blanco I. Role of Alpha-1 antitrypsin in human health and disease. Journal of Internal Medicine. 2014; 276: 311-335.
- Janciauskiene SM, Bals R, Koczulla R, Vogelmeier C, Köhnlein T, Welte T. The discovery of α1-antitrypsin and its role in health and disease. Respiratory Medicine. 2011; 105(8): 1129-1139.
- Karatas E, Di-Tommaso S, Dugot-Senant N, Lachaux A, Bouchecareilh M. Overview of Alpha-1 antitrypsin deficiency-mediated liver disease. EMJ Hepatology. 2019; 7: 65-79.
- National Organization for Rare Disorders (NORD). Rare Disease Database: Alpha-1 antitrypsin deficiency. https://rarediseases.org/rare-diseases/alpha-1-antitrypsin-deficiency/. Published 2017. Accessed Jan. 2020.
- The Childhood Liver Disease Network. Alpha-1-antirypsin deficiency. https://childrennetwork.org/Clinical-Studies/Alpha-1-Antitrypsin-Deficiency. Published 2019. Accessed Jan. 2020.
- Blanco I, Bueno P, Diego I, et al. Alpha-I antitrypsin Pi*Z gene frequency and Pi*ZZ genotype numbers worldwide: an update. Int J COPD. 2017; 12: 561-569.
- Patel D, Teckman J. Alpha-1 antitrypsin deficiency liver disease. Clinical Liver Disease. 2018; 22: 643-655.
- Sandhaus RA, Turino G, Brantly ML, et al. The diagnosis and management of Alpha-1 antitrypsin deficiency in the adult. J COPD Found. 2016; 3(3): 668-682.
- Teckman J, Rosenthal P, Abel R, et al. Baseline analysis of a young α-1-antitrypsin deficiency liver disease cohort reveals frequent portal hypertension. Journal of Pediatric Gastroenterology and Nutrition. 2015; 61(1): 94-101.
- Tanash H, Piitulainen E. Liver disease in adults with severe Alpha-1-antitrypsin deficiency. Journal of Gastroenterology. 2019; 54: 541-548.
- Alpha-1 Foundation. Liver Disease. https://www.alpha1.org/Newly-Diagnosed/Learning-about-Alpha-1/Liver-Disease. Published 2019. Accessed Jan. 2020.
- American Thoracic Society; European Respiratory Society. American Thoracic Society/European Respiratory Society statement: standards for the diagnosis and management of individuals with alpha-1 antitrypsin deficiency. Am J Respir Crit Care Med. 2003; 168(7): 818-900.
- Mayo Clinic. Liver Transplant. https://www.mayoclinic.org/tests-procedures/liver-transplant/about/pac-20384842. Published 2019. Accessed Jan. 2020.
- Larsson C. Natural history and life expectancy in severe alpha-1 antitrypsin deficiency, Pi Z; Acta Medica Scandinavica. 1978; 204: 345-351.